Why Mental Health Policies in India Fail in Practice: The Ground Reality
The Ministry of Health and Family Welfare, Government of India, recently relaunched the National Mental Health Survey after a nine-year hiatus. It aims to gather updated data on policy and programme development, including the prevalence of mental health disorders post COVID, and treatment gaps.
Nikita Joshi
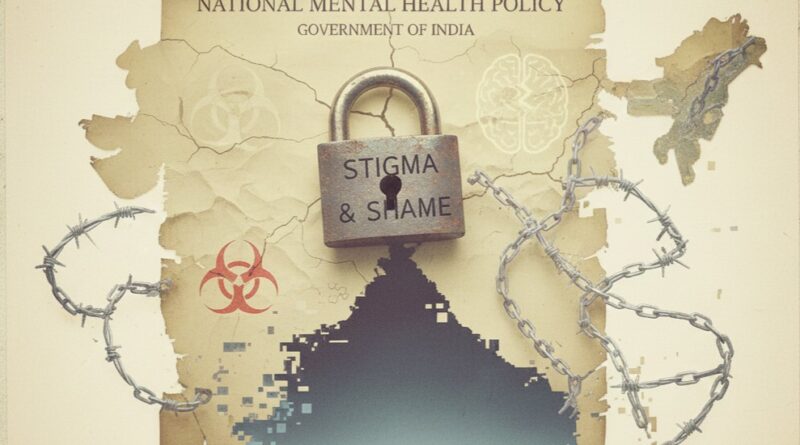
The mental health crisis is one of the many crises India is currently facing. Suffering from mental health disorders is still considered a shame in the country. A viral video of a journalist asking political leaders if they have ever received mental health therapy shows how well-known people are deflecting the question, and somehow not receiving therapy ever is a proud thing to say. This mentality generally results in the gap between the well-written policies on paper and their implementation.
THE GAP: POLICY VS REALITY
The data from the past decade shows that up to 80-90% Indians with mental health conditions never receive proper treatment. The reasons can be varied, from a lack of treatment services to stigma. Another survey revealed that the gap between diagnosis and treatment stands at 95 %. This means that only 5 out of 100 individuals who are diagnosed with mental health illnesses are actually treated. If you go through the Indian Union Budget (2025-2026), only 1.18% was allocated to mental health.
Therefore, it is pretty evident how much importance mental health holds in the eyes of the MoHFW. Less budget allocated to mental health leads to the already existing institutions competing for crumbs. Therefore, new ideas, innovation, and infrastructure keep lagging. Even if on paper, funds do get approved for various mental health projects, such as community care or rural support systems, but they largely end up directed towards hospitals and academic institutes.
PSYCHIATRIST SCARCITY
The gap between policy and reality can never be filled until we have enough psychiatrists. India is currently sitting with a severe shortage of psychiatrists, with 0.75 psychiatrists per 100,000 people. Whereas the WHO recommends 3 psychiatrists per 100,000 people. The global average is about 1.10 per 100,000 people; the average is 10 per 100,000 people in high-income countries.
India neither lacks in population nor in well-informed youth. Therefore, the gap and lack of psychiatrists only point towards their value in the country and unsupportive means and facilities for the study of psychiatry. Even today, there are only 1300-1400 seats available for MD psychiatry for a population of more than 1.46 billion people. This scarcity leads to expensive therapy. It is absolutely unaffordable for economically vulnerable groups. It is not that they do not suffer from mental health illnesses, it’s just that they are obliged to live with this suffering.
People are now aware of their mental health more than ever. It is one of the perks of social media that it helps in spreading awareness about mental health. Social media has served as an open platform to have conversations and discussions on topics that were once stigmatised. Because of this, not only is the public more aware, but it also expects more from the system.
The awareness programmes or the helpline numbers are not enough now, but the real access to treatment matters. A treatment that is effective, easily available, and most importantly, affordable. Now is the time to take mental health seriously. Now is the time to conduct a survey, build stronger policies, and act on them. Now is the time to increase the health budget because one way or the other, this country’s health is getting worse. And only a physically and mentally healthier country will bring all the new possibilities.